What if we could combine technology and medicine to boost the body’s natural ability to fight off life-threatening diseases like cancer — without patients having to undergo harsh treatments like chemotherapy and radiation?
Ambitious questions like this are at the forefront of an innovative research collaboration at UW Medicine, created by Hannele Ruohola-Baker, PhD, the associate director of the Institute for Stem Cell and Regenerative Medicine (ISCRM). She sees artificial intelligence as the future of regenerative medicine and has teamed up with researchers from the Institute for Protein Design (IPD) on a collaboration informally known as DREAM, short for Designed Regeneration for Medicine.
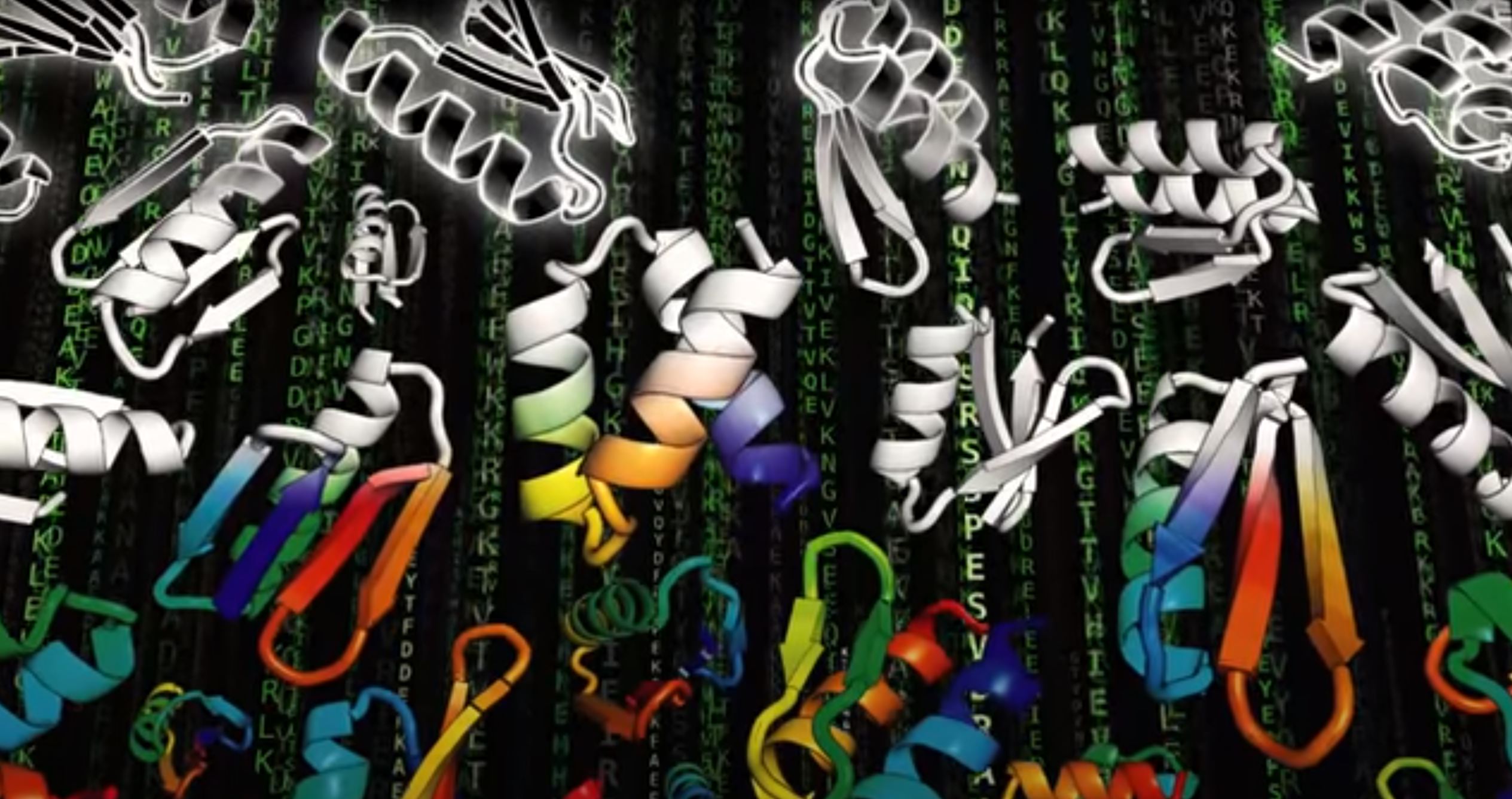
In their shared lab space, located in Seattle’s high-tech South Lake Union neighborhood, ISCRM and IPD researchers are using stem cell biology, protein design and artificial intelligence to develop new treatments for cancer, COVID-19 and other urgent health challenges.
“Artificial intelligence is really entering the space of protein design and biology,” says Ruohola-Baker. “In the next five years, these fields are going to change the future of medicine.”
Collaborating to design better cures

Hannele Ruohola-Baker, PhD
The DREAM collaboration began with an intriguing observation. The Ruohola-Baker lab, which studies stem cell regeneration, noticed something unusual: When they gave fruit flies chemotherapy or radiation, the flies’ cancer cells would die, but the cancer stem cells survived.
They learned that the dying cancer cells send out a distress signal to cancer stem cells, which triggers a cell-to-cell signaling pathway called Tie2. This tells the cancer stem cells to go into a sleep mode that shields them from damage during chemotherapy or radiation. Then, when treatment ends, the cancer stem cells “wake up” and can begin growing and dividing again, leading to a cancer relapse.
Because the Tie2 pathway is also found in human stem cells — both healthy and cancerous — the Ruohola-Baker team wanted to know if they could use protein design to regulate pathways like Tie2, preventing cancer stem cells from entering this protective sleep mode.
They brought their discovery to IPD’s researchers, who suggested using tiny, computer-designed structures called nanocages. These microscopic protein scaffolds are created with powerful computational-design software, which uses artificial intelligence to design synthetic proteins that will snap together into nanocages. The nanocages would bind to Tie2 receptors on a cell’s surface, giving the researchers control over the cell’s activity and the Tie2 pathway.
Working together, IPD designed and ISCRM tested several nanocages that successfully inhibited the Tie2 pathway. By keeping only the cancer stem cells “awake” during treatment, while allowing healthy, noncancerous stem cells to enter protective sleep, scientists can target cancer more effectively and reduce damage to healthy tissues.
Being able to control pathways like Tie2 could also help calm inflammation caused by infection, promote healing by encouraging cell regeneration and even block viral infection before it happens.
“Now, we can take what nature already does and do it better. We’re not just waiting and seeing what happens; we’re really designing this regeneration by designing the proteins,” says Ruohola-Baker.
The DREAM team proved that nanocages can be used to influence cellular pathways in the body, lowering cancer stem cells’ defenses. But just keeping the cancer cells “awake” wasn’t enough — they also needed a more targeted and effective way to kill them. So they decided to take on one of the most aggressive, treatment-resistant cancers around.
WATCH this video to learn how the Institute for Protein Design uses artificial intelligence and computational design to create synthetic proteins that can lead to new medicines.