A winding path to medicine
Dickson grew up in a farming family in Scobey, Montana. As the kid sister tagging along after her much taller big brother, she was nicknamed Mutt, after the old comic strip “Mutt and Jeff.” To this day, it’s the name she prefers to go by.
Dickson’s first career plan was to be a plumber. However, upon receiving a full academic scholarship, she enrolled at Montana State University at Bozeman — only to drop out after two years, when they tried to make her declare a major.
After a brief detour into carpentry, Dickson became a truck driver. The accidents she regularly saw on the road inspired her to train as an emergency medical technician, so she could help care for the injured. During her seven-year career as a paramedic in Las Vegas, she also became a registered nurse.
While on a temporary assignment with the Department of Energy to the Republic of the Marshall Islands, Dickson fell in love with the islands. She returned to work there for three years and became fascinated with the pathology she saw. She decided to become a physician and enrolled at the University of Washington School of Medicine.
Dickson’s first role model in medicine was her childhood family doctor, Dr. Clyde Norman. “He sewed me up on his kitchen table more than once,” she recalls. “I really wanted to be as kind and caring and skilled as Doc Norman.” Like him, she planned to become a family practice physician.
But during medical school, another influential figure sparked her interest in mental health care: Dr. Nicholas Ward, her second-year behavioral medicine professor and later her attending physician during her third-year psychiatric clerkship. Inspired by Ward, Dickson did a combined residency in family medicine and psychiatry at West Virginia University.
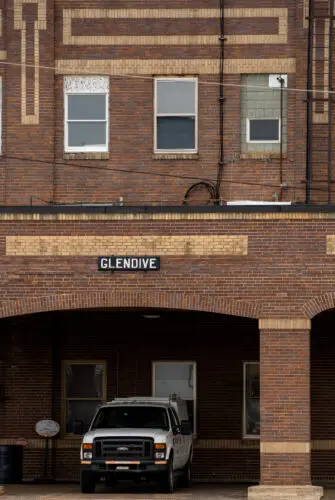
Eventually, Dickson brought her two passions together when she moved to Glendive, in eastern Montana, where she is in private solo practice as a general family practitioner and a psychiatrist — both of which the community desperately needed.
Expanding mental health care in rural communities
Montana has the second-highest suicide rate in the nation, according to the Centers for Disease Control and Prevention. Some of the most frequently cited causes are rural isolation and economic stress on farmers. In addition, Montana has a high percentage of veterans, so post-traumatic stress disorder (PTSD) and depression are common.
In 2002, Dickson became the founding director of the psychiatric unit at Glendive Medical Center. But after four years, she was burned out. Every night, she says, she would get calls from emergency rooms or law enforcement agencies from one of the 17 counties in the region, expecting her to help them handle a suicidal person. She resigned in 2006. Unable to bring enough providers to their isolated town, the medical center was forced to close their psychiatric unit for several years, and anyone needing mental health care had to travel several hours to a larger city.
Today, Glendive Medical Center has reopened with several therapists on staff, which eases the burden in the area. While she doesn’t think COVID significantly affected mental health in her community, because most people didn’t alter their routines, Dickson says she’s noticed other changes in the community’s overall mental health since the pandemic.
“I would say the changes now are even greater financial pressure on farmers and ranchers,” says Dickson. “The suicide rate has probably stayed the same — and probably always will, while we fight the rural stigma of mental illness and easy access to alcohol and guns.”
One bright spot is that telemedicine is beginning to transform mental health care throughout rural America. Dickson spends 20 hours a week providing outpatient psychiatric care at the Montana Veterans Administration (VA) community clinic, about 85% of which is done remotely via video call. Although she prefers face-to-face conversations, Dickson acknowledges that telehealth consultations help to meet the urgent and ever-growing need statewide.
“The rewarding part of the VA work is helping someone with their PTSD or depression, understanding as best I can what they’re going through and what struggles they have daily as a result of their meritorious service to the country,” Dickson says.