In addition to making UW Medicine more competitive on the research scene, the eye institute will make life better for patients. After surgery, patients will receive post-operative care at one site, rather than needing to visit different sites in the UW system. It’s a function of having all the subspecialties under one roof.
Deborah Lam, Res. ’06, acting instructor of ophthalmology, is delighted with the change. “This will improve continuity of care,” she says.
Comprehensive patient care also extends to trauma and injury. Housed at Harborview, the region’s only level I trauma center, the eye institute has a dedicated ophthalmological trauma service. For instance, Lam, the first director of Trauma Services, is on call five nights a week.
In addition to trauma care, the institute offers a number of other clinical services — including those provided by Tueng Shen, associate professor of ophthalmology, director of the Refractive Surgery Center, and the Northwest Lions Foundation Professor in Cornea and External Disease.
Shen performs refractive surgery, cataract surgery, and corneal transplant surgery using donor tissue. In addition, she performs special corneal surgery using an artificial cornea called the Boston Keratoprosthesis, developed by Claes Dohlman, her mentor at Harvard Medical School. Shen, who established the artificial cornea program at UW Medicine in 2004, is one of the few surgeons trained to perform the transplant of this artificial cornea.
Most of Shen’s patients are from Washington, Wyoming, Alaska, Montana, or Idaho (the region served by the UW School of Medicine), but she hopes, one day, to cast a wider net — to help more of the estimated 12 million people who have some form of corneal blindness, many in the developing world, where the health-care infrastructure makes corneal surgeries and post-operative care all but impossible. For those patients, says Shen, “the current model does not cut it.”
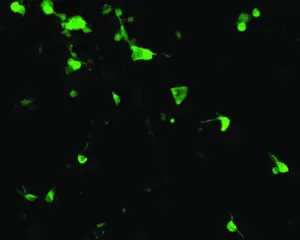
In an attempt to address these limitations, Shen’s research group is developing the next generation of artificial corneas for the global market. With her background in medical engineering, she and her colleagues in bioengineering and electrical engineering are designing biopolymer and wireless microelectronic systems that are customized for controlled medication release and post-operative monitoring. “Our goal is to create high-tech and low-cost solutions to treat blindness worldwide,” she says.