A 20-year-old woman falls headfirst into a tree while snowboarding, waking up in a hospital to discover she can’t move her arms or legs, control her bowel or bladder, or breathe on her own without a ventilator.
A 20-year-old woman falls headfirst into a tree while snowboarding, waking up in a hospital to discover she can’t move her arms or legs, control her bowel or bladder, or breathe on her own without a ventilator.
She’ll be on a long road to recovery and will have many medical needs that require attention from a large team of experts — which is exactly the kind of multidisciplinary care that UW Medicine’s inpatient rehabilitation unit provides.
As a rehabilitation physician, Jamie Ott, DO, acting assistant professor of rehabilitation medicine at the UW School of Medicine, helps ensure patients remain medically stable so they can participate in therapy. This could mean managing health conditions like diabetes or heart failure, caring for injury complications like infection or helping to manage a person’s pain. But there are many other roles and expertise needed on a rehabilitation care team, she says.
In the snowboarder’s case, for example, a speech therapist might evaluate her swallowing, thinking and cognition. A respiratory therapist would help wean her from the ventilator and then downsize her tracheostomy tube. An occupational therapist would help her relearn activities for daily living, like going to the bathroom, getting dressed and eating without assistance. A physical therapist would help her with mobility and balance tasks, like using a wheelchair or transferring herself from the bed to a chair. And the entire medical team, nurses and doctors, would help ensure all her bodily systems are running smoothly, says Ott.
“It’s not always apparent to people the diverse expertise that a large team brings to a patient’s care,” says Deborah Crane, MD, MPH, associate professor of rehabilitation medicine at UW School of Medicine, medical director of inpatient rehabilitation and chief of service for rehabilitation medicine at Harborview Medical Center.

Jamie Ott, DO

Deborah Crane, MD, MPH

Charles Bombardier, PhD, ABPP

After a collision while playing hockey left Marc with six broken vertebrae, his road to recovery began at Harborview’s inpatient rehabilitation clinic. “From the nurses to the doctors, the physical therapists and the occupational therapists, my care at Harborview was great,” says Marc. “We saw people from all walks of life there, many of them with no insurance, and they were getting the same treatment that I was. I think that’s pretty powerful.”
UW Medicine’s inpatient rehabilitation unit is spread across two locations: UW Medical Center – Montlake and Harborview Medical Center. Patients often require three to eight weeks of inpatient care before transitioning to an outpatient setting, and need inpatient rehabilitation for many reasons, including spinal cord injury, stroke, traumatic brain injury, amputation and burn injury.
As the only Level 1 burn and trauma center in our region, Harborview provides the most comprehensive care for the most complex rehabilitation patients and turns no one away because of income level or insurance status. For these reasons, there is a wide diversity of patients who receive care, something faculty members value.
“We see patients who live in Seattle and struggle with day-to-day housing, but we also see patients who are engineers at Google or are returning to work in corporate America,” says Ott. “We see patients from Eastern Washington and more rural areas as well as across state lines who are flown in because they need specialty trauma care at Harborview.”
Another key aspect of a person’s recovery can involve overcoming significant mental barriers. “In the background, there’s a whole adjustment process. There’s grieving and loss. There’s adjusting to disability,” says Charles Bombardier, PhD, ABPP, professor of medicine in the Division of Rehabilitation Psychology and Neuropsychology.
As a rehabilitation psychologist who has worked at UW Medicine for over 30 years, Bombardier has helped many people overcome psychological barriers to participating in their own rehabilitation. Sometimes this involves treating people for depression, anxiety, pain, addiction or sleep problems.
Often, he focuses on changing a person’s behaviors. For instance, people with spinal cord injuries must learn new ways of moving so they don’t get pressure sores; people who have had strokes need to make lifestyle changes to decrease their chances of having another stroke; and people with brain injuries may need cognitive behavioral therapy to treat depression and help them find pleasant meaningful activities in their lives.
Besides a full team of experts on a person’s care team, Bombardier points out another reason that makes UW Medicine so unique. Most clinicians at UW Medicine are also scientists, which means they not only treat patients but also conduct research that will improve the care of their patients.
Bombardier is one of those physician-scientists and is presently researching ways of decreasing pain using hypnosis along with cognitive therapy. The results of his clinical trial look promising; he and his team have been able to reduce pain intensity for patients who are already receiving medical treatment, with effects that last after treatment stops.
“We’ve done medication studies, we’ve done therapy studies, we’ve done exercise studies. And our patients get a chance to participate in this research,” says Bombardier. “Investing in the University of Washington is investing in the future of rehabilitation because we are literally creating and testing the next therapies that will help patients do better.”
Crane agrees that investing in the inpatient rehabilitation unit makes a big difference. There is almost always a need for state-of-the-art equipment, such as exoskeletons, body-weight-supported walking devices and virtual reality systems that can augment therapy, since these often aren’t covered by grants or insurers.
She also points out that the rehabilitation program has been ranked* among the top five in the nation for many years. Investment would allow expansion of services in both inpatient and outpatient settings and the creation of new treatments, which will improve patient outcomes.
When it comes down to what motivates them day in and day out, Crane, Bombardier and Ott all agree, it’s about helping people live their fullest lives, finding inspiration in people’s strength and resilience and working with a great team. “It’s everyone working together and pulling together for the patient — and the patient being part of the team,” says Bombardier.
Written by Eleanor Licata
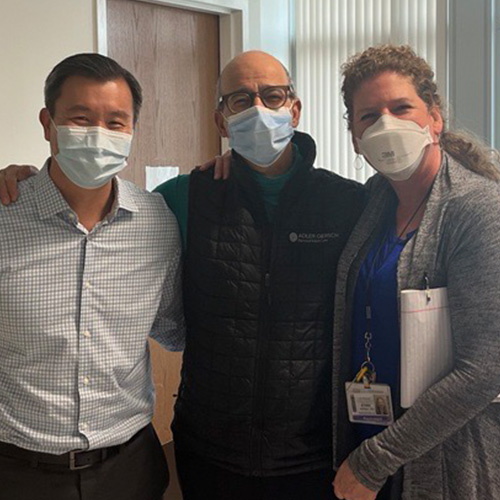
Attorneys Richard H. Adler, along with his law partners (Melissa D. Carter, Arthur D. Leritz, and Steve J. Angles) and staff at the law firm Adler Giersch, have generously supported the UW Medicine Department of Rehabilitation Medicine since 2009. And, for the past seven holiday seasons, they’ve purchased needed supplies and equipment, so care teams can continue to provide the best care possible for their patients.
Help our multidisciplinary care teams improve patient recovery with a gift to the Rehabilitative Medicine Discretionary Fund.
*UW Medicine – University of Washington Medical Center has been ranked among the top five in the nation for rehabilitation medicine by US News & World Report for more than 15 years.